Osteoarthritis of the shoulder is a chronic disease that develops on the basis of cartilage damage, leading to the appearance of bone growth and limited mobility. Most often, the elderly suffer from pain, but hard physical labor and inflammatory processes contribute to the early development of the pathology. Without prompt treatment, movement in the affected joint is completely blocked.
General information
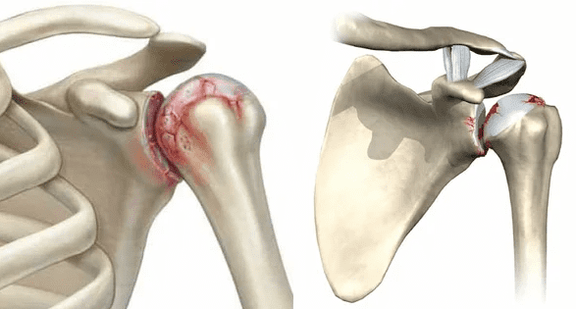
Cartilage is a smooth layer between the exposed areas of bone. It ensures easy sliding relative to each other, ensuring the joint works freely and painlessly. Excessive stress, inflammation, or trauma can trigger a gradual degenerative process that spreads over the entire surface.
As a result, the smoothness of the joint surface is disturbed and movements begin to cause pain. At the same time, bone begins to appear along the edges of the joint, replacing the affected cartilage. As the degenerative process progresses, it involves not only the bones but also the surrounding tissues. The limbs are deformed, the muscles are stiff, the ligaments are weak and lose their elasticity. If left untreated, the patient will lose the ability to move the arm.
View
Depending on the developmental etiology, primary and secondary arthropathy are distinguished. The primary form occurs spontaneously, often in the context of an overburdened joint. Secondary is caused by a third-party pathology, such as trauma, intense inflammatory processes, metabolic disorders, etc. v. Both forms of the disease are similar in symptoms.
The reasons
Unlike the knee, ankle, and hip joints, the shoulder is not subject to significant stress while walking, which is why this form of arthritis occurs much less often. Illness can be caused by:
- frequent excessive physical activity: weight lifting, professional sports, vibration;
- Congenital abnormalities of the shoulder joint structure and adjacent structures;
- rheumatoid arthritis, systemic lupus erythematosus and other autoimmune diseases;
- congenital weakness of the connective tissue, accompanied by increased mobility of the joints;
- trauma: dislocation, sprain and rupture of ligaments, fracture in the joint;
- hormonal changes and disruptions (including pregnancy, menopause);
- inflammatory diseases of the joints and periarticular structures (arthritis, bursitis, etc. );
- metabolic disorders, including gout, diabetes mellitus.
An important role in predisposition to joint disease is genetics.
Degree
Doctors determine 3 degrees of deformity of the shoulder joint, determine its symptoms and choose treatment tactics:
- Grade 1 is characterized by minimal manifestations: pain occurs only with intense or prolonged exertion and passes quickly after rest, and X-ray shows subchondral sclerosis of the joint surface;
- with grade 2 arthritis, the pain becomes much stronger, the patient has to take pain relievers to relieve the pain; X-rays show markedly narrowed joint space, extensive areas of cartilage destruction, as well as bone (osteogenesis) growth;
- Grade 3 disease with constant severe pain, significantly limited joint mobility, complete destruction of cartilage tissue, deformation of the bone structure, and a large number of osteoblasts.
The symptoms
The main symptoms of shoulder arthritis include:
- pain: arising from a decrease in the smoothness of the joint surface, the growth of osteoblasts and bone deformation; intensity, duration and nature of sensations depend on the extent of the injury;
- crunching sound: one of the characteristic symptoms of the disease, which appears in the early stages; differs from physiology in a coarser tone, and is also often accompanied by pain;
- limited mobility: associated with the appearance of pathological growths and destroyed cartilage particles inside the joint; in the early stages, manifested by slight stiffness in the morning, then gradually increased to the point of complete immobility (stiffness);
- deformity: a change in the contour of first only the joint, then the hand, which occurs in the late stages of the disease and shows complete destruction of cartilage and involvement of bones, muscles, and ligaments in thepathological process.
Progression of symptoms can take years, even decades, but eventually fibromyalgia leads to inability to move the arm and severe pain.

Diagnose
Diagnosis of shoulder osteoarthritis requires an integrated approach. To accurately diagnose and determine the extent of damage, doctors use the following methods:
- questioning and taking history: patient complaints are recorded, cases of occurrence of certain symptoms are identified; without fail, information about past illnesses and injuries, the presence of joint damage in parents is clarified;
- examination: the doctor visually assesses the joint, determining range of motion, areas of greatest pain, etc. v . . . ;
- X-ray and CT: the main diagnostic methods allow you to see the characteristic symptoms of osteoarthritis (narrowing of joint space, cartilage degeneration, bone growth and deformity);
- Ultrasound: helps to evaluate the condition of cartilage, bones, ligaments, joint capsule and muscles;
- MRI: allows you to obtain virtual slices of all the structures of the affected area;
- laboratory diagnosis: blood tests reveal an active inflammatory process, which often accompanies arthritis;
- arthroscopy: examining the joint from the inside with a camera inserted through a small puncture.
If the disease is of a secondary nature, examination and consultation of a narrow specialist on the underlying pathology is mandatory.
Shoulder joint treatment
Treatment of shoulder osteoarthritis depends on the extent of damage: in stages 1 and 2, the disease can be successfully cured or delayed thanks to the right selection of drugs. With extensive destruction, the only way to restore mobility and complete pain relief is surgery - arthroscopy with "cleaning" of the joint.
Medicines for treatment
Medical treatment of shoulder osteoarthritis is aimed at reducing symptoms and restoring cartilage tissue. For this, the following groups of drugs are used:
- non-steroidal anti-inflammatory drugs: suppress inflammatory reactions and relieve pain; available in the form of tablets, ointment, suppositories and in the form of injections;
- hormonal agents (corticosteroids): used when NSAIDs are ineffective, have similar effects; a good effect is provided by long-acting drugs, which are injected directly into the joint cavity;
- antispasmodics, vitamin B: used to relieve muscle spasms inevitably associated with advanced joint disease;
- chondroprotectors: designed for long-term use, aimed at restoring cartilage tissue;
- drugs that improve microcirculation: indirectly stimulate the regeneration process by improving the blood supply to the affected area;
- Enzyme blockers: partially slow down the destruction of cartilage tissue.
The choice of specific drugs, dosage, frequency of use and duration of the course is made solely by the doctor! It's important to remember that over-the-counter medications can cause faster joint degeneration and other side effects.
Physical therapy
Physiotherapy techniques and physiotherapeutic exercises significantly facilitate the course of the disease and enhance the effect of drugs. The following procedures have been shown to work well:
- acupuncture therapy: relieve pain, reduce inflammation, improve microcirculation and stimulate cartilage tissue regeneration;
- shock wave therapy: exposure to sound waves of a certain frequency contributes to the destruction of bone-forming cells, facilitating movement in the affected joint;
- electrophoresis, phonophoresis: delivery of drugs (analgesics, chondroprotectors) into tissues using electrical impulses or ultrasound; promote better drug absorption;
- Massage exercises and physiotherapy: dose loading on joints and intense manual activity stimulates blood circulation in tissues.
Like medications, physical therapy, massage, and exercise should be prescribed and performed under the supervision of a specialist. If in the quiet period they are beneficial, then the action against the background of the acute inflammatory process can cause increased pain.
Surgery
The final stage of shoulder osteoarthritis is accompanied by severe symptoms and requires surgical treatment. Most of the changes that occur as a result of degeneration are irreversible, which is why the only way to restore mobility to a person is through an endoscopy. The affected joint is replaced with a modern prosthesis that takes over its full functions. This surgery is especially effective in young and middle age, as it allows you to live pain-free for many years.
Preventive
Like any joint disease, shoulder osteoarthritis is easier to prevent than to cure. Orthopedists recommend observing the following rules:
- eliminate or minimize occupational risk factors (vibration, weight lifting);
- not to let go of motivation, but also not to strive for sports records: it is better to choose a moderate training option;
- nutrition and weight control;
- undergo regular inspections to identify possible problems.
Diet
With any degree of shoulder osteoarthritis, it's important to monitor your nutrition:
- avoid overeating and being overweight;
- minimize harmful products: fatty, spicy, salty, alcohol, canned food, smoked meat;
- eat adequate amounts of foods rich in collagen (jelly meat, aspic) and omega-3s (fatty fish, olive oil);
- give preference to boiled, steamed or stewed foods over fried foods;
- reduce the amount of fast-digesting carbohydrates.
The diet should be complete and include the necessary amount of vitamins, minerals and nutrients.
Consequences and complications
Even a mild pain and crackle in the shoulder can turn into unpleasant consequences. If left untreated, dry joints lead to:
- significant limitation of mobility up to ankylosing spondylitis (bone fusion);
- severe pain even at rest;
- Severe deformity of the shoulder and the entire arm.
To avoid these problems, it is important not to search the internet for how to cure shoulder osteoarthritis with folk remedies, but simply to contact a chiropractor for therapy options.
Treatment in specialized clinic khám
It is not possible to cure arthritis on its own. The specialists of the modern clinic provide patients with complex treatment methods for shoulder osteoarthritis:
- modern drug treatment regimens combine high efficiency and few side effects;
- new and time-tested physical therapy techniques;
- PRP therapy;
- physical therapy exercises and massage to reduce limited joint mobility.
If necessary, medical punctures of the joint are made with the introduction of pain medication or artificial synovial fluid to facilitate movement.
We monitor the patient throughout the treatment to keep the disease under control.
Benefits of a modern clinic
Specialized blades offer their patients:
- comprehensive health screening programs;
- extensive tests for accurate diagnosis;
- consultation of narrow specialists of many different profiles;
- modern treatment regimens, which include not only drugs, but also physiotherapy, massage and exercise;
- Reasonable prices for all services.
Osteoarthritis of the shoulder is a problem that can completely change a person's life. Do not let the disease turn into an irreversible stage, see an orthopedist.





































